Immediate Conversation Starters: Breaking the Silence with Grace
- "I might not understand exactly how you feel, but I am here to sit in the dark with you for as long as you need."
- "I love you, and nothing about your struggle changes the way I see you or your value."
- "You don't have to explain anything or perform for me; just being in the same room is enough."
- "I noticed you've been carrying a heavy weight lately, and I want you to know I'm not going anywhere."
- "I’m bringing over dinner at 6 PM. I’ll leave it on the porch, or I can come in and eat with you—no pressure either way."
- "I miss your presence, but I want you to take all the time you need to heal."
- "Your feelings make sense given what you're going through, and you aren't 'too much' for me."
- "I’m not here to fix this, I’m just here to love you through it."
- "What is one small thing I can do today that would make your life even 1% easier?"
- "I believe in you, even on the days when you don't believe in yourself."
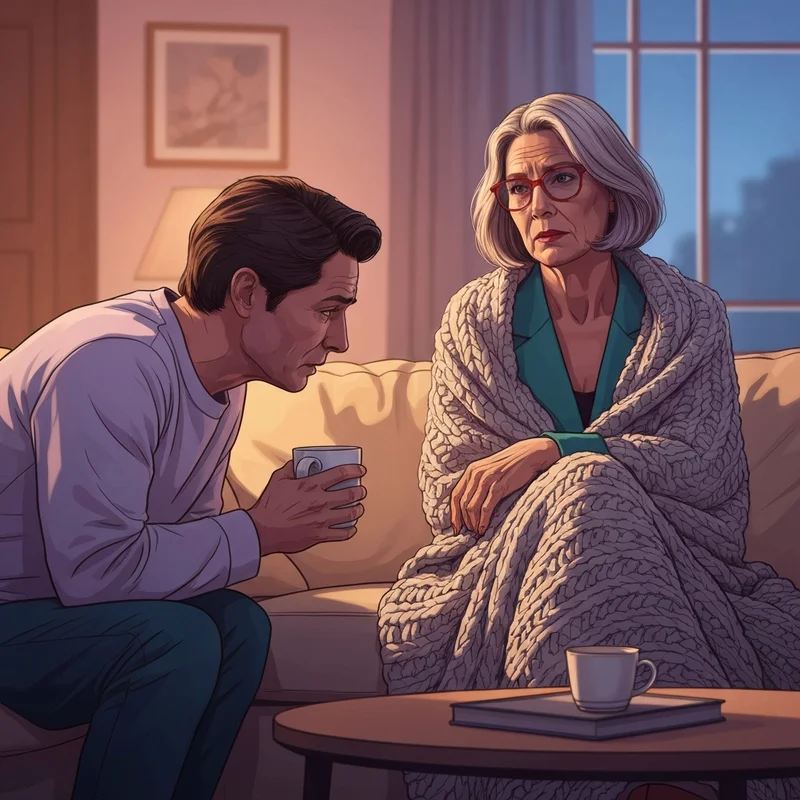
The air in the room feels thick, almost stationary, as you sit across from someone you love. You see the way their gaze lingers on the floor, the subtle slump in their shoulders that speaks of an exhaustion sleep cannot touch. You want to reach out, to pull them back into the light, but the fear of saying the wrong thing—of pushing them further into that gray fog—paralyzes you. This is the shadow pain of the supporter: the desperate desire to be a lifeline while feeling like you're drowning in your own helplessness. When we consider what to say to people with depression, we are really looking for a bridge across the silence. Psychology tells us that depression is profoundly isolating, a condition that whispers to the sufferer that they are a burden. By choosing words that emphasize presence over performance, you dismantle that lie. You aren't just giving them a phrase; you are offering a sanctuary where they don't have to hide their pain to keep your friendship.
Texting Scripts: How to Check In Without Being Overwhelming
- "Just a little 'I love you' text. No need to reply, just wanted you to see it."
- "I saw this meme/video and thought of you. Sending some low-pressure smiles your way."
- "Thinking of you today. I’m around if you want to vent, or if you just want someone to be on the other end of the phone in silence."
- "I’m heading to the store—do you need more coffee, laundry detergent, or snacks? I’ll drop them by later."
- "Checking in on my favorite person. How is your heart feeling today?"
- "No pressure to talk, but I’m going for a walk later. I’d love for you to join, but I totally get it if today isn't the day."
- "I’m so proud of you for just existing today. I know it’s hard."
- "Sending you a virtual hug and a reminder that you are deeply important to me."
- "I’m here for the long haul. You don't have to get better on a schedule for me."
- "Hey, I’m free all Sunday. If you want me to come over and just help with the dishes or watch a movie, just say the word."
Digital communication is a unique tool for supporting someone with depression because it removes the immediate demand for eye contact and verbal processing, which can be draining during a depressive episode. The goal of these texts is to provide 'low-friction' connection. When someone is in the depths of a low period, even a text notification can feel like a demand for energy they don't have. By explicitly stating 'no need to reply' or 'no pressure,' you give them the gift of being seen without the debt of a response. This mechanism relies on the psychological principle of consistent availability—proving through small, repeated actions that your support is unconditional. It’s like a soft hum in the background of their life, reminding them that the world hasn't forgotten them, even when they feel invisible.
The Art of Validation: Moving Beyond 'Fixing'
Validation is the act of acknowledging a person's internal experience as valid and understandable, even if you haven't lived it yourself. In the context of mental health support, it is the opposite of 'toxic positivity.' When we tell someone to 'look on the bright side' or 'be grateful,' we inadvertently shame them for their symptoms. Instead, focus on reflective listening. If they say, 'I feel like a failure,' a validating response is, 'I can see how heavy that feeling is for you right now, and I’m so sorry you’re carrying it.' You aren't agreeing that they are a failure; you are agreeing that their feeling of being a failure is real and painful. This distinction is vital for maintaining trust.
Physically, when you are engaging in these conversations, aim for 'soft' body language. Sit at an angle rather than directly across, which can feel confrontational. Maintain a gentle, steady voice. The sensory environment matters—dim the lights, offer a warm drink, and allow for long pauses. Silence isn't a void to be filled; it is space for them to find their words. By validating their pain, you are practicing active listening, which studies from organizations like the Mayo Clinic suggest is the single most effective way to help a loved one feel supported. You are creating a 'holding environment,' a psychological term for a safe relationship where a person can disintegrate and rebuild without judgment.
Say This vs. Not That: A Decision Matrix for Empathy
| If they say... | Instead of saying (Avoid)... | Try saying (Better)... | Why it works |
|---|---|---|---|
| "I can't get out of bed today." | "You just need some fresh air!" | "I hear you. It sounds like your body needs rest right now." | Validates physical symptoms without judgment. |
| "I’m such a burden to everyone." | "Don't be silly, you're fine." | "I’m here because I want to be, not because I have to be." | Reassures them of your agency and love. |
| "I don't think I'll ever feel better." | "Everything happens for a reason." | "It’s terrifying to feel stuck. I’m holding onto hope for both of us." | Acknowledges their despair while offering a tether. |
| "I don't want to talk about it." | "But I’m trying to help you!" | "I respect that. I’m happy to just sit here in the quiet with you." | Prioritizes their boundaries over your ego. |
| "Everything is just too much." | "Think about people who have it worse." | "It sounds like you're at your limit. What can I take off your plate?" | Acknowledges their reality instead of comparing pain. |
Comparing their pain to others or offering unsolicited advice is a common reflex because we want the person to stop hurting. However, these responses often backfire. Depression is not a lack of perspective; it is a clinical condition. When you use the 'Better' column, you are shifting from being a 'fixer' to being a 'companion.' This shift is crucial for [primary keyword] because it centers the sufferer's needs. The 'Why it works' column highlights the mechanism of agency—allowing the person with depression to guide the pace of the support. This builds their confidence and reduces the shame often associated with being 'the one who needs help.'
Practical Acts of Service: Lending Your Energy
- "I’m going to the grocery store. Give me a list of 5 things you need, and I’ll drop them off."
- "I have an hour free on Tuesday. I’d love to come over and fold your laundry or take the trash out while you nap."
- "Can I help you research some therapists or look into what your insurance covers?"
- "I’m ordering takeout for myself—what’s your favorite order so I can send some your way?"
- "I’d love to take your dog for a walk this afternoon to give you some quiet time."
- "I’m happy to be your 'boring' buddy—I’ll come over and do my own work while you do yours, no talking required."
- "If you have any phone calls or appointments you've been putting off, I can sit with you while you make them."
- "I noticed your car needs gas/wash; can I take it for a quick spin to handle that for you?"
- "I’m bringing over a 'care package' with your favorite tea and those fuzzy socks you like."
- "Would it be helpful if I checked in on you every morning at 10 AM, or is that too much?"
Depression often manifests as 'executive dysfunction,' making simple tasks like doing the dishes or making a phone call feel as exhausting as climbing a mountain. This is where practical help becomes a form of profound emotional support. Instead of asking 'Let me know if you need anything'—which puts the burden of planning on the depressed person—offer specific, limited choices. This reduces the cognitive load required to accept help. When you offer to fold laundry or bring groceries, you are reducing the external chaos that often mirrors their internal state. This is a manifestation of 'social support theory,' which suggests that tangible aid significantly reduces the impact of stress and mental illness.
Caring for the Caregiver: Setting Boundaries
Supporting someone with depression is a marathon, not a sprint. It is incredibly easy to experience 'compassion fatigue,' where you feel drained, resentful, or hopeless yourself. To be a sustainable source of support, you must maintain your own boundaries. This might mean saying, 'I love you and I want to hear this, but I only have 20 minutes to talk right now because I need to decompress.' This isn't being selfish; it’s being responsible. If you burn out, you can't help anyone.
Remember that you are a friend, not a therapist. While your support is invaluable, it cannot replace professional intervention. Part of [primary keyword] is knowing when to gently pivot toward clinical help. You might say, 'I’ve noticed how much you’re struggling lately, and I wonder if talking to a professional might give you some extra tools that I simply don't have.' Frame it as an addition to your support, not a replacement for it. You are still their 'Bestie,' their safe harbor, but even a harbor needs a lighthouse. By taking care of yourself, you model the very self-care and boundary-setting that your loved one may eventually need to practice for their own recovery.
Encouraging Professional Support: The Bridge to Healing
- "I’ve noticed you haven't been feeling like yourself lately, and I’m concerned because I care about you. Have you thought about talking to someone?"
- "I know finding a doctor is a huge chore. If you want, I can sit with you while we look through the list together."
- "There is no shame in getting extra support. It’s like going to a doctor for a broken leg."
- "If you're worried about the first appointment, I can drive you there and wait in the car or the lobby."
- "I found a few highly-rated therapists who specialize in what you're feeling. Would you like to see the list?"
Encouraging professional help is one of the most delicate parts of supporting someone with depression. The key is to avoid sounding like you are 'diagnosing' them or trying to 'get rid' of them. Use 'I' statements to express your concern and focus on the impact their symptoms are having on their quality of life. According to resources like Mind, offering to help with the logistics of therapy can be the deciding factor for someone who feels overwhelmed by the healthcare system. You are acting as a bridge, helping them navigate the gap between their current pain and the help they deserve. Always reinforce that seeking help is a sign of strength and resilience, not weakness.
When to Seek Emergency Help: Safety First
If you ever feel that your loved one is in immediate danger of hurting themselves or someone else, the priority shifts from conversation to safety. Do not leave them alone. If you aren't with them, stay on the phone while you or someone else contacts emergency services or a crisis hotline. It is better to have a friend who is temporarily upset with you for calling for help than to lose that friend forever. Signs of a crisis include talking about wanting to die, giving away prized possessions, or a sudden, eerie calm after a long period of deep depression.
You are doing an incredible thing by showing up. It’s okay to feel nervous, and it’s okay if your voice shakes when you speak. The fact that you are looking for what to say to people with depression shows that you have the empathy and heart necessary to make a difference. Healing isn't linear, and your words are seeds. Some will sprout immediately, and others might take time, but they are all part of the garden of recovery. If you ever need to practice these conversations, Bestie’s Roleplay feature is here to help you find your footing in a safe space. You’ve got this, and they are lucky to have you.
FAQ
1. What do you say to someone with depression?
When talking to someone with depression, focus on validation and presence. Standalone summary: Effective communication involves acknowledging their pain without trying to 'fix' it immediately. Start with phrases like 'I'm here for you' or 'It's okay not to be okay.' Avoid offering unsolicited advice or telling them to 'snap out of it,' as this can increase feelings of shame.
2. How to start a conversation about depression?
To start a conversation about depression, choose a quiet, private moment. You might say, 'I've noticed you've been a bit down lately, and I wanted to check in. How are you really doing?' Use open-ended questions and let them know you're asking because you care, not because you're judging their behavior.
3. What should I not say to someone with depression?
Avoid phrases that dismiss their experience, such as 'It's all in your head,' 'Just be positive,' or 'Others have it worse.' These comments can make the person feel misunderstood and isolated. Instead, focus on listening and offering practical support.
4. How to support a friend with severe depression?
Supporting a friend with severe depression requires patience and consistent presence. Offer to help with daily tasks, encourage them to seek professional help, and let them know you're there for the long haul. Most importantly, familiarize yourself with crisis resources in case of an emergency.
5. What to text someone who is depressed?
When texting someone who is depressed, send low-pressure messages like 'Thinking of you' or 'No need to reply, just sending love.' This lets them know they're on your mind without demanding they use limited emotional energy to respond.
6. How to help someone with depression who doesn't want help?
If someone with depression doesn't want help, remain a supportive presence without pushing. You can say, 'I respect that you're not ready for help right now, but I'm still here whenever you are.' Continue to check in and offer low-stakes connection.
7. What are signs someone is struggling with depression?
Common signs of depression include persistent sadness, loss of interest in hobbies, changes in sleep or appetite, social withdrawal, and verbalizing feelings of hopelessness. If you notice these patterns, it may be time to initiate a gentle check-in.
8. How to validate someone's feelings of depression?
To validate feelings of depression, acknowledge the reality of their pain. Use phrases like 'I can see how hard this is for you' or 'It makes sense that you feel overwhelmed.' This shows you are listening and that their feelings are valid.
9. What is the best way to encourage professional help?
Encourage professional help by framing it as an additional resource for their well-being. Say something like, 'I've noticed you're carrying a lot, and I wonder if a therapist could help lighten the load. I'm happy to help you find someone if you'd like.'
10. How to be a good listener for mental health?
Being a good listener for mental health means giving the person your full attention, avoiding interruptions, and reflecting back what they've said. Use 'I' statements and maintain a non-judgmental stance throughout the conversation.
References
mayoclinic.org — Depression: Supporting a family member or friend
nhs.uk — How to help someone with depression
mind.org.uk — Helping someone with depression
helpguide.org — How to Help Someone with Depression