The Silent Panic of the Delivery Room
It starts as a low hum in the back of your mind the moment the test turns positive—not a hum of excitement, but a vibration of sheer, unadulterated dread. While other people are browsing nursery themes, you are staring at your reflection in the mirror, feeling like a passenger in a body that has suddenly become a ticking clock. This isn't just 'nerves' or the standard jitters of a first-time parent; this is the visceral, heart-pounding reality of fear of pregnancy at its most clinical level.
For those living with this condition, the thought of the transition phase or the physical mechanics of labor feels less like a miracle and more like a psychological siege. You might find yourself searching for an exit strategy before the journey has even truly begun. The weight of societal expectation tells you to 'trust your body,' but your mind is screaming for a controlled, predictable alternative.
Giving birth with tokophobia is a unique challenge that requires moving beyond traditional breathing exercises into the realm of medical strategy and psychological shielding. It is about reclaiming your agency in a process that feels inherently out of your control. To move beyond the paralyzing fear and toward a functional plan, we must first look at the clinical frameworks that allow for choice in the delivery room.
Can You Choose a C-Section Due to Fear?
Let’s look at the underlying pattern here: your fear is not a failure of character, but a clinical data point that deserves a seat at the table during your obstetric care for tokophobia. Historically, the medical community prioritized vaginal birth above all else, often dismissing maternal anxiety as something to be 'managed' rather than accommodated. However, the ethical landscape has shifted significantly toward recognizing mental health as a valid indication for surgical intervention.
According to the American College of Obstetricians and Gynecologists (ACOG), a 'Cesarean Delivery on Maternal Request' (CDMR) is a recognized pathway. This means that even in the absence of a traditional medical emergency like placenta previa, your psychological well-being can be the primary driver for a planned cesarean for mental health. You have permission to prioritize your psychological safety just as much as your physical safety.
Choosing this path while giving birth with tokophobia is a logical response to a phobic trigger. It transforms an unpredictable, potentially traumatic event into a scheduled, highly regulated medical procedure. This shift in perspective may help reduce the 'anticipatory trauma' that often plagues the third trimester. You aren't 'taking the easy way out'; you are selecting the clinical tool best suited to preserve your mental integrity during a major life transition.
Advocating for Your Mental Health in the Hospital
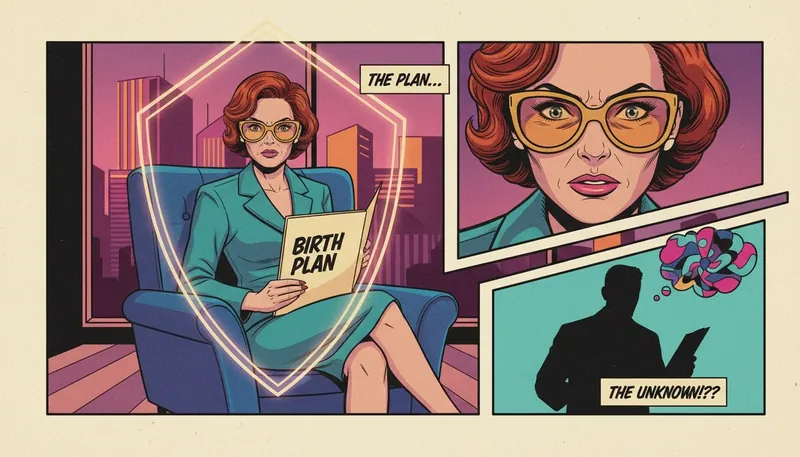
In the medical world, if you aren't the one holding the map, you’re just a passenger on someone else’s route. When you are giving birth with tokophobia, your primary objective is to convert your internal panic into a professional, non-negotiable strategy. This starts with your birth plan for anxiety disorders, which should be treated as a legal-medical directive rather than a 'wish list.' You need to be the CEO of your delivery room, ensuring every nurse and resident who walks through that door knows exactly where the boundaries lie.
Here is the move: Do not ask for permission to be afraid. State your needs as clinical requirements. If you encounter an OB who suggests you 'just try for a natural birth first,' that is your signal to escalate or switch providers. Your advocacy must be high-status and high-clarity. Managing fear in the delivery room isn't about being 'nice'; it's about setting a perimeter around your psyche.
Use this script when discussing childbirth options for tokophobics: 'I have a clinical diagnosis of tokophobia, and for the preservation of my mental health and to prevent postpartum PTSD, I am requesting a maternal request cesarean for phobia. I need to know today if this facility can support a trauma-informed surgical birth plan, or if I need a referral to a provider who specializes in high-anxiety deliveries.' This places the responsibility on the provider to meet a clinical standard of care.
The Reality of the Room: Sedation and Anesthesia
Let’s cut through the fluff and perform some reality surgery on what actually happens when you’re giving birth with tokophobia in a surgical setting. The biggest lie you've been told is that you have to be 'present' and 'zen' for every second of the process. If your phobia is triggered by the sensation of being cut or the loss of lower-body control, we need to talk about the fact sheet of anesthesia. You aren't being 'weak' for wanting to feel nothing; you’re being practical.
For a planned C-section, you'll typically receive a spinal block. You’ll be awake, but numb from the chest down. If the thought of being awake while people move around behind a blue curtain makes you want to crawl out of your skin, you need to discuss 'gentle sedation' options with the anesthesiologist beforehand. While total general anesthesia is rare for elective cases due to safety risks for the baby, there are anti-anxiety medications (like midazolam) that can be administered the second the baby is out to stop a panic attack in its tracks.
He didn't 'forget' to tell you about the risks; medical teams often downplay the sensory triggers of the OR because they see them every day. But for you, the smell of antiseptic and the sound of monitors is a minefield. Demand a 'silent OR' or bring noise-canceling headphones. If you are giving birth with tokophobia, your goal is to minimize sensory input. This isn't a spa day; it's a medical procedure. Treat it with the same detached, clinical focus that the doctors do, and you’ll find the exit door much faster.
FAQ
1. Can I be denied a C-section if I have tokophobia?
While doctors have the right to refuse a procedure they deem medically unnecessary, ACOG guidelines suggest that if a provider cannot meet a maternal request for a C-section, they should refer the patient to a doctor who will. Your mental health is a valid clinical reason for the procedure.
2. How do I explain tokophobia to my doctor?
Use clinical language. Instead of saying 'I'm scared,' say 'I experience pathological fear of childbirth that interferes with my daily functioning.' Mention that you are seeking 'obstetric care for tokophobia' to ensure your birth plan for anxiety disorders is prioritized.
3. Does an elective C-section increase the risk of postpartum depression?
Actually, for those with severe tokophobia, a planned C-section can reduce the risk of birth-related PTSD and postpartum depression by providing a sense of control and preventing the trauma of an emergency intervention during a panicked labor.
References
acog.org — ACOG: Cesarean Delivery on Maternal Request
mother-ly.com — Motherly: Understanding Tokophobia