The 3 AM Fog: When Joy Feels Heavy
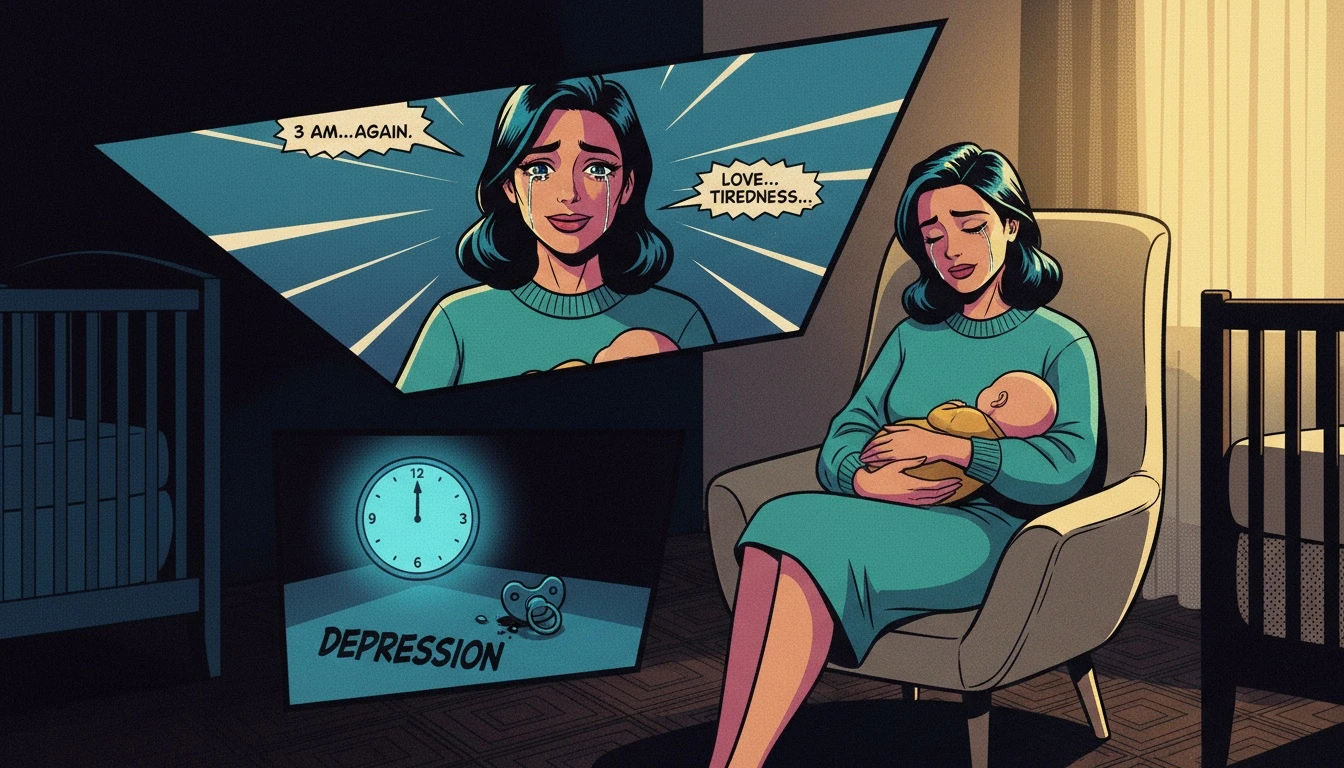
It is 3:14 AM, and the nursery is filled with the rhythmic, mechanical hum of the white noise machine and the faint, sweet scent of milk and unwashed hair. You are holding the miracle you prayed for, yet a heavy, inexplicable sob is caught in your throat. This isn't the 'glow' promised in the magazines. Instead, you are navigating intense pregnancy emotional changes that have followed you across the threshold of birth.
The transition into motherhood is often romanticized as a seamless ascent into bliss, but for many, it feels more like a visceral descent into a foreign emotional landscape. You might find yourself crying because the toast is cold or because the sunset feels too beautiful to bear. Understanding the difference between baby blues and postpartum depression starts with acknowledging that your brain is currently a construction site, undergoing massive structural and chemical renovations while you are still trying to live inside it.
The Day 3 Hormone Dump: Cory’s Biological Blueprint
Let’s look at the underlying pattern here: what you are experiencing isn't a failure of will; it is a biological inevitability. Within the first 24 to 48 hours after delivery, your levels of estrogen and progesterone plummet back to pre-pregnancy levels. This is known as hormonal withdrawal postpartum, and it is one of the most significant endocrine shifts a human body can endure. This 'crash' is the primary engine behind after birth mood swings, often resulting in the 'Baby Blues' that affect up to 80% of new parents.
According to the National Institute of Mental Health, these 'Blues' typically peak around day three to five and dissipate within two weeks. It is a state of hyper-reactivity, not a clinical pathology. You are re-calibrating your neurochemistry after ten months of expansion.
The Permission Slip: You have permission to feel absolutely miserable while simultaneously being grateful for your child. Your hormones do not require your moral approval to fluctuate.
To move beyond the biological 'why' and into the practical 'what,' we must shift our lens from the mechanics of the body to the specific signals of the mind.
Red Flags: When It’s Not Just 'The Blues'
Let’s be real: 'Baby Blues' is a cute name for a temporary storm, but it stops being cute when the storm refuses to break. If you are three weeks out and you still feel like you’re underwater, we need to talk about postpartum mood disorders. The difference between baby blues and postpartum depression is found in the duration, the intensity, and the 'flavor' of the darkness. While the blues make you weep, PPD makes you feel numb, trapped, or even resentful.
Perinatal psychiatric disorders aren't just 'sadness.' They manifest as postpartum anxiety symptoms—the racing heart, the intrusive thoughts of harm, the terrifying 'what-ifs' that keep you from sleeping even when the baby finally does. It’s not just 'new mom nerves'; it’s a clinical hijacking. If you find yourself unable to bond, or if the fatigue feels like a lead blanket you can't kick off, that’s not a phase. That’s a medical emergency dressed in yoga pants.
To move from identifying the crisis to managing the outcome, we must shift from a state of observation to a state of strategic defense.
The Strategic Support Net: Pavo’s Postpartum Move
In any high-stakes environment, survival depends on the strength of your infrastructure. New mom mental health is not a solo project; it is a logistical operation. If the data suggests that you are sliding from the blues into a more serious territory, we don't wait for 'rock bottom.' We mobilize. This is about reclaiming your agency through strategy.
1. The Tactical Script: Don't wait for your partner to guess your needs. Use this: 'I am experiencing symptoms of a postpartum mood disorder. I need you to handle the midnight-to-4 AM window so I can get four hours of uninterrupted sleep, which is non-negotiable for my recovery.'
2. The Clinical Outreach: Contact your OB-GYN or a therapist specializing in perinatal care immediately. Use the term 'postpartum anxiety symptoms'—it signals to them that you have done the work and need professional intervention, not just a nap.
3. The Delegation Tier: Identify three 'low-stakes' tasks you can outsource (laundry, grocery orders, dog walking). This isn't laziness; it's resource management.
FAQ
1. How long do baby blues typically last compared to PPD?
The baby blues usually start within a few days of birth and resolve on their own within two weeks. Postpartum depression can start anytime in the first year and requires professional treatment to resolve.
2. Can I have both anxiety and depression after birth?
Yes. Many women experience a blend of postpartum anxiety symptoms and depressive moods, often referred to as a perinatal mood and anxiety disorder (PMAD).
3. Does having the baby blues mean I will get PPD?
Not necessarily. While they share some symptoms, the baby blues are a common response to hormonal withdrawal postpartum, whereas PPD is a distinct clinical condition involving more severe biochemical imbalances.
References
nimh.nih.gov — NIMH: Perinatal Depression
en.wikipedia.org — Wikipedia: Postpartum depression