Distinguishing Between NPD and Bipolar Disorder
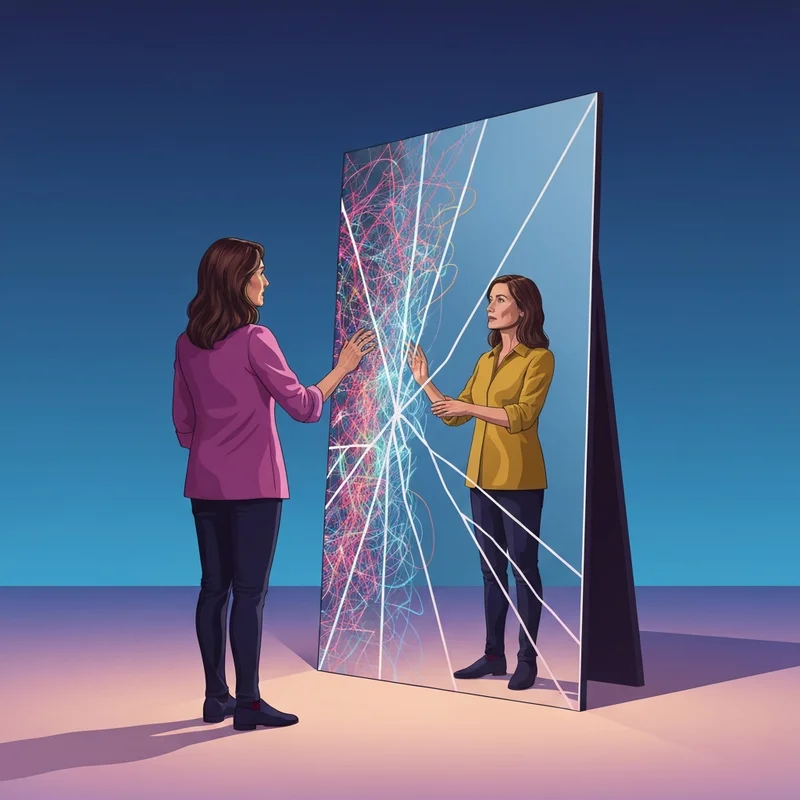
Understanding the overlap of npd and bipolar disorder is the first step toward regaining your peace. While they may look similar during a crisis, they have fundamentally different origins. Bipolar disorder is primarily a mood disorder characterized by shifts in energy and biological regulation, whereas narcissistic personality Disorder (NPD) is a stable personality structure rooted in self-image and relational patterns. When you are standing in the middle of a storm, it feels like the same rain, but knowing if it is a seasonal surge or a permanent climate change determines how you build your shelter. You are not alone in this confusion; thousands of partners and individuals seek this clarity every single day.
Imagine sitting across from someone you love at 2 AM. Their eyes are bright, their words are moving at a hundred miles an hour, and they are describing a world-changing plan that seems entirely detached from reality. You feel a familiar tightening in your chest—a mix of excitement for their joy and a cold, creeping dread. Is this a manic episode where they need medical support and stabilization, or is this the height of narcissistic grandiosity where your role is merely to provide applause for their ego? The air in the room feels electric but thin, and you realize you have been holding your breath for months, waiting for the other shoe to drop.
This distinction matters because the path to healing is different for each. Bipolar disorder often responds remarkably well to mood stabilizers and clinical intervention, as it addresses the neurochemical imbalances driving the 'highs' and 'lows'. In contrast, narcissistic traits are deeply ingrained patterns of relating to the world that require long-term, specialized psychodynamic work. Recognizing these nuances allows you to stop blaming yourself for 'not being enough' to stabilize their mood. You are the partner, not the clinician, and your primary responsibility is to maintain your own emotional health while navigating these complex waters.
The 5% Factor: Understanding Comorbidity
When we look at npd and bipolar disorder together, we find a specific intersection often called 'The Manic Narcissist' in informal circles. This occurs when an individual meets the criteria for both, or when their manic episodes specifically mimic the grandiosity found in NPD. According to Psychology Today, about 5% of individuals may actually carry a dual diagnosis. This comorbidity creates a 'perfect storm' where the biological energy of mania fuels the psychological need for narcissistic supply, making it incredibly difficult for loved ones to set boundaries or even hold a grounded conversation.
| Feature | Bipolar Mania | Narcissistic Grandiosity |
|---|---|---|
| Duration | Episodic (days to weeks) | Persistent and stable over years |
| Root Cause | Biological/Chemical shifts | Defensive self-image structure |
| Empathy | May fluctuate with mood | Consistently impaired or selective |
| Reaction to Feedback | Can be irritable or euphoric | Fragile; often leads to 'narcissistic rage' |
| Sleep Needs | Significantly reduced without fatigue | Generally normal unless obsessed |
| Sense of Self | Inflated but often fluctuates | Rigidly superior regardless of reality |
In a clinical setting, recent research (2022) emphasizes that while the 'highs' look similar, the underlying mechanism of 'hypomania' in bipolar II can sometimes be mistaken for the high-functioning arrogance of NPD. The key is often found in the 'lows'. A person with bipolar disorder typically experiences a crash into deep, often debilitating depression that is clearly distinct from their manic state. A person with NPD may experience 'narcissistic injury' or deflation, but it is often characterized more by bitterness and external blame than the heavy, biological weight of clinical bipolar depression.
De-escalation Script Library
Communicating when npd and bipolar disorder are present requires a specific set of tools. You cannot use standard logic during a manic peak or a narcissistic defensive spike. Instead, you must use 'De-escalation Scripts' that prioritize your safety and emotional distance. These scripts are not about 'winning' the argument; they are about exiting the conflict loop without triggering a more severe episode. When a partner is in a state of elevated grandiosity, they are seeking a specific reaction—either total submission or a fight that justifies their anger. By refusing both, you reclaim your power.
- Scenario: They are making impulsive, expensive plans.
Script: "I can see you're really excited about this. Let's write down the full plan today and review the budget together on Tuesday before taking any action." - Scenario: They are blaming you for their current mood.
Script: "I hear that you're frustrated right now, but I'm not able to accept responsibility for your feelings. I'm going to step into the other room while we both calm down." - Scenario: They are demanding constant praise or attention.
Script: "I appreciate the work you've put into this. Right now, I need some quiet time to recharge so I can be fully present with you later." - Scenario: They are speaking rapidly and ignoring your input.
Script: "It feels like we're moving very fast. I'm going to take a 20-minute break from this conversation so I can process what's been said." - Scenario: They are using 'gaslighting' to shift reality.
Script: "We clearly have different memories of how that happened. I'm not going to argue about the past; I'm focused on what we do next." - Scenario: They are in a 'rage' cycle.
Script: "I cannot continue this conversation while there is shouting. I am leaving the house for an hour and will check back when things are calmer." - Scenario: They are refusing to discuss treatment.
Script: "I care about you and our relationship. My boundary is that we need a professional plan in place for us to move forward safely together." - Scenario: They are experiencing a 'crash' and seeking pity.
Script: "I see that you're hurting. I can sit with you for a little while, but I also need to make sure I'm taking care of my own needs today."
Using these scripts feels awkward at first because they are 'ego-neutral'. You aren't feeding the fire, but you aren't trying to blow it out with your own breath either. This approach is grounded in the psychological principle of 'Gray Rocking'—becoming as uninteresting as a gray rock to someone seeking an emotional reaction. When dealing with npd and bipolar disorder, this technique preserves your energy and prevents the 'circular arguments' that lead to total exhaustion.
Safety Boundaries & Rule-Setting
Setting boundaries when dealing with npd and bipolar disorder is not an act of aggression; it is an act of self-preservation. Because both conditions can involve a lack of insight into how one's behavior affects others, you must be the one to define the 'rules of engagement'. These boundaries must be clear, consistent, and—most importantly—enforced by you. A boundary without a consequence is just a suggestion, and in the world of personality and mood disorders, suggestions are often ignored.
- Financial Protection: Maintain a separate bank account and set a hard limit on 'impulse spending' that triggers an automatic freeze or discussion.
- Treatment Non-Negotiables: Medication adherence and regular therapy sessions must be a condition of the relationship's intimacy.
- Communication Hours: No 'heavy' or 'confrontational' discussions after 9 PM, as sleep deprivation can trigger manic episodes and heighten irritability.
- Physical Space: Have a designated 'safe zone' in the home or a plan to stay with a friend when a manic or narcissistic rage episode begins.
- No-Gaslighting Rule: If reality is being denied, you exit the conversation immediately rather than trying to 'prove' your side.
- Social Safety: You have the right to leave any event or gathering if their behavior becomes erratic or embarrassing to you.
Implementing these rules will likely cause initial pushback. Someone with NPD may view these boundaries as a 'challenge' to their control, while someone in a manic state may see them as an unfair 'restriction' on their freedom. Stay firm. Your mental health is the foundation upon which your life is built. If that foundation cracks, you cannot help them, and you certainly cannot help yourself. It is helpful to remember that you are setting boundaries with the behavior, not the person. This distinction helps reduce the guilt that often comes with protecting yourself from someone you love.
A Simple Plan for Today: Partner Recovery
The weight of loving someone with npd and bipolar disorder often leads to what clinicians call 'Caregiver Burnout' or 'Compassion Fatigue'. You spend so much time monitoring their moods—checking the weather of their soul before you even decide if you can speak—that you lose track of your own needs. This hyper-vigilance is a trauma response. Your brain has learned that to stay safe, it must be the world's leading expert on their psychology. But who is the expert on yours?
In our 'A simple plan for today' approach, we focus on returning the gaze to yourself. This isn't about being 'selfish'; it's about basic survival. If you are constantly pouring into a vessel that has a hole in the bottom (as narcissistic structures often do), you will eventually run dry. Real recovery for the partner involves de-coupling your worth from their stability. Whether they choose to take their medication today or whether they choose to acknowledge your feelings, you must decide that your day will still contain at least one element of joy that is entirely independent of them.
- Morning grounding: Spend 5 minutes in silence before checking their 'vibe' for the day.
- External support: Call one friend today and talk about your life, not theirs.
- Physical movement: Walk for 15 minutes to process the cortisol and adrenaline that builds up during high-conflict episodes.
- Creative outlet: Spend time on a hobby that they have no part in and no influence over.
According to Healthline, the chronic stress of these relationships can lead to physical health issues for the partner. This is why we must treat your wellness as a priority, not an afterthought. You are allowed to be happy even if they are currently in a cycle. You are allowed to have a peaceful evening even if they are restless. Reclaiming this autonomy is the most powerful thing you can do for the health of the entire dynamic.
Safety Check: When to Seek Professional Help
One of the hardest questions to answer is when the situation has become unsalvageable. When npd and bipolar disorder are both present, the potential for 'emotional volatility' is high. If the individual refuses to acknowledge the impact of their behavior or consistently weaponizes their diagnosis to avoid accountability, the relationship enters a toxic territory. You cannot 'love' someone out of a personality disorder, and you cannot 'reason' someone out of a manic episode. If they are not an active partner in their own treatment, you are not in a partnership; you are in a hostage situation.
When things feel unsafe, it is time to look at the 'Safety Check' list. This isn't about judgment; it's about clear-eyed reality. If you find yourself checking these boxes, it is a signal that professional intervention—and potentially a separation—is necessary for your survival.
- Physical violence or the threat of violence (this is an absolute deal-breaker).
- Consistent financial ruin that threatens your ability to house or feed yourself.
- The use of 'suicide threats' as a method to control your movements or decisions.
- Complete isolation from your friends and family due to their demands or jealousy.
- A total refusal to seek or maintain medical treatment for over six months.
- Your own mental health has deteriorated to the point of depression or chronic anxiety.
Seeking help from a domestic violence resource or a specialized therapist is a sign of strength, not failure. You have fought a long, hard battle, and recognizing the limits of your influence is a profound act of wisdom. The future is still yours to write, and it can be a future defined by peace rather than constant crisis management. Navigating npd and bipolar disorder is a marathon, but you don't have to run it alone.
FAQ
1. Can someone have both NPD and bipolar?
Yes, it is possible for an individual to be diagnosed with both Bipolar Disorder and Narcissistic Personality Disorder (NPD). This is known as comorbidity. While Bipolar is a mood disorder and NPD is a personality disorder, they can coexist, often making the symptoms of both more intense and harder to treat.
2. What is the difference between narcissistic mania and bipolar mania?
The main difference lies in duration and empathy. Bipolar mania occurs in episodes that have a beginning and an end, often followed by depression. Narcissistic grandiosity is a stable, lifelong personality trait. Additionally, during bipolar mania, a person may still feel empathy, whereas NPD typically involves a consistent deficit in empathy.
3. How to deal with a bipolar narcissist partner?
Dealing with a partner who has both requires strict boundaries and 'Gray Rock' communication. You must separate the person from the behavior and ensure that your own safety and financial independence are prioritized. Encouraging medical adherence is key, as treating the bipolar symptoms can sometimes reduce the intensity of narcissistic outbursts.
4. Are bipolar people more narcissistic?
Not necessarily. While people in a manic state may act in ways that seem narcissistic—such as being self-centered or grandiose—these are symptoms of the mood episode, not their permanent personality. Once the mania subsides, a person with bipolar disorder typically returns to their baseline level of empathy and self-awareness.
5. Does bipolar cause narcissistic behavior?
Bipolar disorder does not 'cause' NPD, but a manic episode can cause 'narcissistic-like' behaviors. The chemical surge during mania creates a sense of invincibility and heightened ego. However, true NPD is a separate condition rooted in early development and personality structure rather than temporary brain chemistry shifts.
6. What are the symptoms of NPD vs bipolar hypomania?
NPD traits are ego-syntonic, meaning the person feels their behavior is justified and correct. Bipolar hypomania is often ego-dystonic over time, where the person may later feel regret or confusion about their actions during the episode. NPD involves a constant need for admiration, while hypomania is defined more by high energy and decreased need for sleep.
7. Can bipolar disorder be mistaken for narcissism?
Yes, misdiagnosis is common. A clinician might see the grandiosity of a manic episode and mistake it for NPD, or they might see the entitlement of NPD and mistake it for a mood swing. A long-term clinical history is usually required to see if the symptoms are 'episodic' (Bipolar) or 'pervasive' (NPD).
8. Is NPD and bipolar comorbidity common?
Comorbidity is relatively rare, with studies suggesting about 5% of those with Bipolar Disorder also meet the criteria for NPD. However, the overlap of symptoms makes it appear more common than it is in a formal clinical sense.
9. What is the treatment for NPD and bipolar comorbidity?
Treatment usually involves a combination of mood stabilizers for the bipolar component and specialized psychotherapy (like DBT or psychodynamic therapy) for the narcissistic traits. Managing the mood disorder is often the first priority to create enough stability for the personality work to begin.
10. How to set boundaries with a bipolar narcissist?
Set boundaries by identifying specific behaviors you will no longer tolerate, such as shouting or financial irresponsibility. Communicate these boundaries calmly and during a period of stability. Always have a clear consequence, like leaving the room or the house, and follow through every single time.
References
healthline.com — Bipolar and Narcissism: Tendencies and Symptoms
psychologytoday.com — The Relationship Between Narcissism and Bipolar Disorder
pubmed.ncbi.nlm.nih.gov — Diagnostic concerns and conceptual overlaps: Bipolar and NPD