The Weight of the Hospital Chair
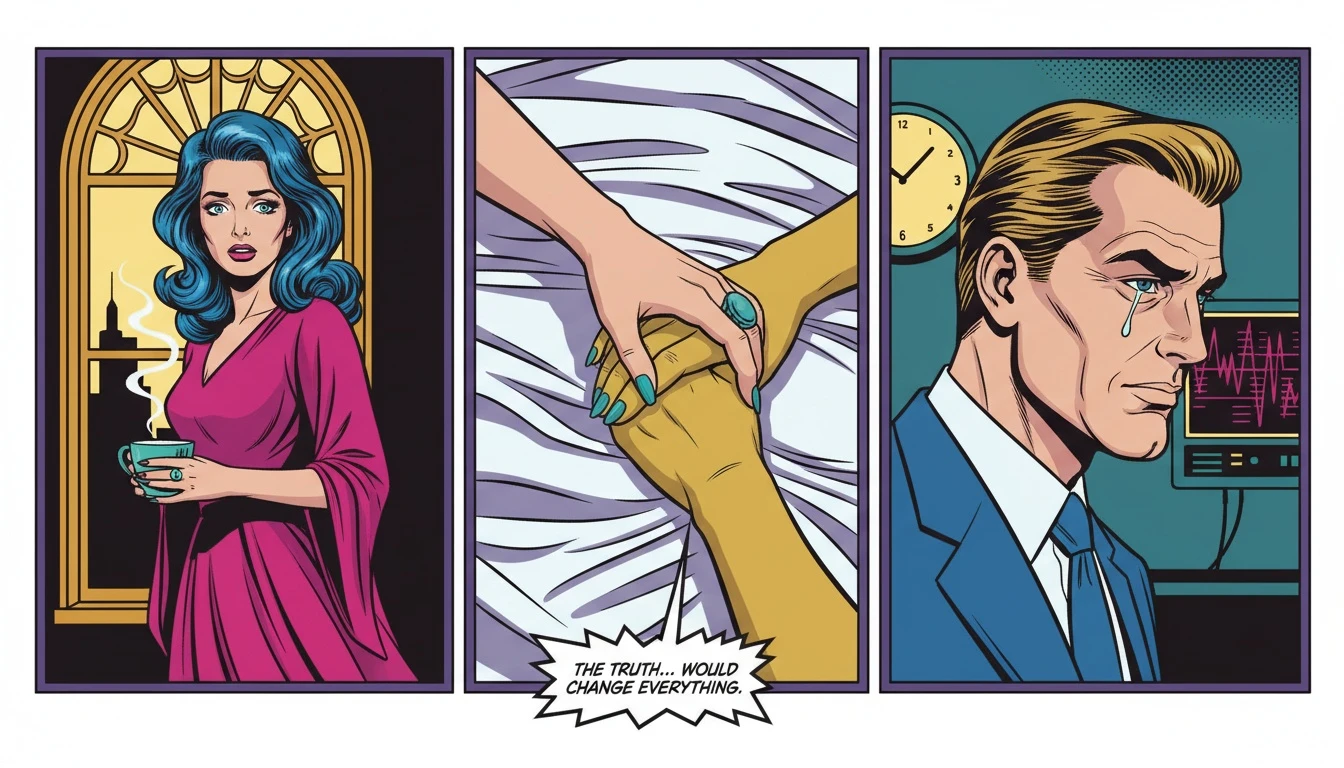
It’s the silence that gets you first. Not a peaceful quiet, but a heavy, waiting silence, punctuated by the rhythmic beep of a machine you can’t identify. The air smells sterile, a clean that feels cold, and the chair you’re sitting in is impossibly uncomfortable. Your own body aches with a sympathetic tension as you watch your loved one, diminished by bandages and tubes, resting in the hospital bed.
In these moments, the world shrinks to the size of this room. You feel a desperate urge to do something, to fix it. But there is nothing to fix. This is the raw, terrifying, and profoundly helpless space of bearing witness to trauma. It’s a space where a simple question—what now?—can feel like an unanswerable void. Knowing how to support a trauma survivor isn't about having a magic wand; it's about learning to sit in that uncomfortable chair with unwavering presence.
First Response: What to Do (and Not Do) in the Immediate Aftermath
Let’s take a deep breath together. Right here, right now. The overwhelm you’re feeling is not a sign of weakness; it’s a testament to your love. That fear coiled in your stomach? That’s your brave heart wanting to protect someone precious. As our emotional anchor Buddy always reminds us, the first step is to validate the emotion—both theirs and yours.
In these early days, your presence is more powerful than any present you could buy. Forget grand gestures. Focus on being a calm, steady harbor in their storm. This is less about finding the perfect thing to say and more about listening. One of the kindest answers to 'what to say to someone in the hospital' is often, 'I'm here. You don't have to talk, but I'm right here.'
Practical help for a recovery patient is a language of love in itself. It’s handling the flood of well-meaning text messages. It’s bringing their favorite worn-in sweatshirt from home. It's making sure there's a cup of tea, just the way they like it, on the bedside table. These small acts of service create a bubble of safety, communicating without words that you see them, you’re with them, and you’re handling the small stuff so they can focus on the monumental task of healing. This is the foundational layer of learning how to support a trauma survivor.
The Long Road: Navigating the Emotional Rollercoaster of Recovery
Once the initial crisis subsides, the real work begins. And it is messy. As our analyst Cory would point out, 'Recovery is not a straight line; it’s a spiral.' There will be days of surprising progress followed by days of deep frustration, anger, or despair. This is not a failure. It is the natural, chaotic rhythm of a nervous system trying to heal itself.
Understanding the psychological mechanics is key to providing long-term support for trauma victims. Your loved one might be irritable, withdrawn, or emotionally volatile. According to the American Psychological Association, these are common trauma responses. Seeing these moments not as personal attacks but as symptoms of their injury is a profound act of compassion. This perspective is vital when helping a family member recover from an accident.
Your role shifts from crisis manager to patient observer. Celebrate the microscopic victories: the first time they sit up on their own, a flicker of their old humor, the moment they ask what’s for dinner. These are the building blocks of their return to themselves. Cory offers this permission slip for all caregivers: 'You have permission to not have the answers. Your job is to be a stable presence, not a perfect problem-solver.' Embracing this truth is a crucial part of knowing how to support a trauma survivor for the long haul.
Don't Forget Your Own Oxygen Mask: A Caregiver's Survival Plan
Let’s be brutally honest: you cannot pour from an empty cup. Sustaining this level of care requires a strategy, not just good intentions. As our pragmatist Pavo insists, 'Hope is not a plan.' Ignoring your own needs is the fastest path to caregiver burnout, which helps no one. Your well-being is not a luxury; it is a critical component of their recovery infrastructure.
We need to address the risk of secondary trauma for caregivers. Constantly being exposed to another's pain can take a significant toll on your own mental health. Building a sustainable plan is non-negotiable. Here is the move:
Step 1: Delegate Ruthlessly. Make a list of tangible tasks (groceries, laundry, walking the dog, updating family) and assign them. When people offer vague help, give them a specific job. Pavo's go-to script: 'Thank you so much for offering. What would be a huge help is if you could manage a meal train for us on Tuesdays and Thursdays. Would that be possible?'
Step 2: Schedule Your Own Recovery. Block out non-negotiable time in your calendar for yourself, even if it’s just 20 minutes to walk outside or listen to music. This isn't selfish; it’s strategic refueling.
Step 3: Set Loving Boundaries. Learning how to help without being overbearing is also about protecting your energy. It's okay to say, 'I can sit with you for an hour, but then I need to go home and rest.' Clear boundaries prevent resentment and ensure the support you give is genuine, not grudging. This strategic self-preservation is the advanced curriculum in how to support a trauma survivor effectively.
FAQ
1. What is the most important thing to remember when supporting a trauma survivor?
The most crucial elements are patience and presence. Your role is not to 'fix' their pain but to create a safe emotional space where they can heal at their own pace. Active listening is far more valuable than giving unsolicited advice.
2. How do I handle their anger or frustration during recovery?
Try not to take it personally. Anger and frustration are often normal and valid parts of processing a traumatic event. Acknowledge their feelings with statements like, 'I can see how frustrating this is,' without trying to solve the problem. This validation can de-escalate the emotion.
3. How can I avoid caregiver burnout?
To avoid caregiver burnout, you must intentionally prioritize your own well-being. This includes setting clear boundaries, accepting concrete help from others, delegating tasks, and scheduling regular time for yourself to rest and recharge away from the caregiving role.
4. What are some practical ways to help besides emotional support?
Practical help can be a lifeline. Consider organizing a meal train, helping with household chores, managing communication with concerned friends and family, providing transportation to appointments, or simply ensuring their recovery space is calm, clean, and comfortable.
References
apa.org — Tips for caregivers of trauma survivors